Researchers Are Developing a Paper Test for Ebola and Other Viruses
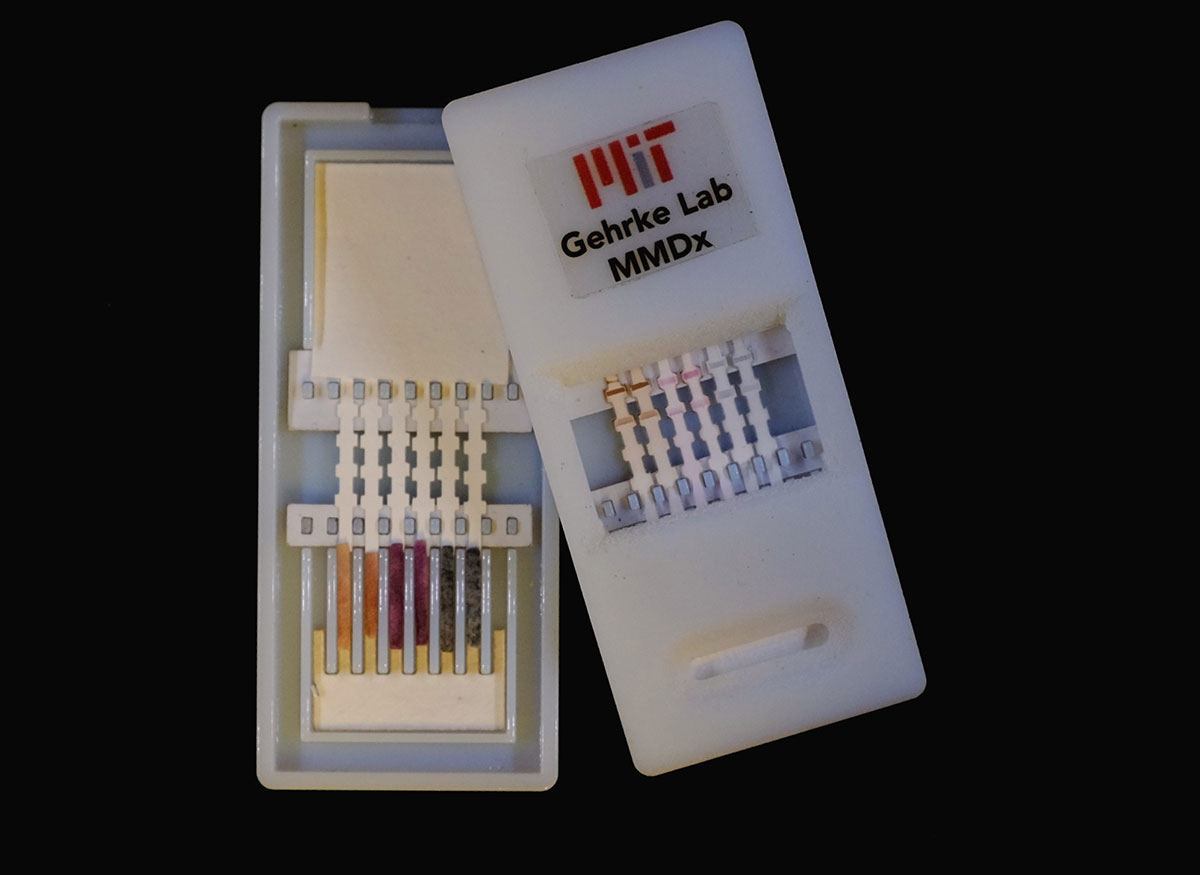
the paper strips in this device can detect ebola, dengue, and yellow fever. photo provided to bostonmagazine.com.
In 2014, West Africa faced the largest Ebola outbreak in history. Skyrocketing diagnosis rates and an alarming number of deaths—the latest CDC figures confirm that nearly 9,600 people have lost their lives in the ongoing crisis—has forced the world to take a hard look at our own preparedness for such an event. Now, engineers and biomedical scientists from MIT and Harvard Medical School (HMS) are working on something that may help put us all at ease: a diagnostic paper test.
Researchers have developed a small, paper test for Ebola and other viruses that are characterized by a fever by using gold nanoparticle sensors that can quickly identify pathogens. Lee Gehrke, a professor at both MIT and HMS who is leading the research team, says that the device is designed to work like a pregnancy test. According to an HMS report, results can be obtained in less than 20 minutes.
“After applying a sample of blood, serum, or urine to the device, the liquid flows along a paper-like material that is striped with antibodies–proteins that can pick out and attach to a single type of molecule out of a very complex mixture, as you would find in blood.” Gehrke explains. “A second antibody that is connected to tiny gold nanoparticles also attaches to the virus or viral protein in the blood sample. While flowing through the paper, the gold nanoparticles accumulate at the stripe if a virus is present, forming a band that you can see by eye.”
In addition to detecting Ebola, Gehrke says that this “multiplexed device” is designed to screen for other viruses such as dengue fever, Marburg fever, and the Chikungunya virus. The idea, he says, is to create a diagnostic tool that can help healthcare providers rapidly determine if a patient’s fever is the result of one of these viruses or a symptom of a less serious condition.
Though the worst of the current Ebola outbreak appears to be behind us, Gehrke says the development of these tools will help to prepare for future crises. In addition to developing a device that can detect multiple viruses, he says that researchers are also designing a test that can be modified based on location and the “type of threat.” Though researchers cannot yet say when the device will be available commercially, they anticipate that its final retail cost will be $10 or less.
“Without being alarmist, it is important to recognize that the United States needs to have strategies for surveillance that will identify dangerous viruses. The mosquito that carries dengue fever is already widely distributed in the continental U.S., and a new virus called Chikungunya—also carried by mosquitoes—is an emerging threat to our southern neighbors. The American West is home to dangerous hantaviruses that are spread by aerosolized rodent urine and feces,” Gehrke says. “Our device can be used in the U.S. both as a surveillance tool to monitor areas for the presence of viruses, and also as a diagnostic tool for rapidly evaluating patients who present with fevers of unknown origin.”

